On 17 November 2020, the World Health Organization (WHO) formally launched the Global Strategy to Accelerate the Elimination of Cervical Cancer. The International Agency for Research on Cancer (IARC) is supporting this WHO initiative by providing key evidence, technical materials, and updates for policy-makers, programme managers, and experts implementing the Global Strategy.
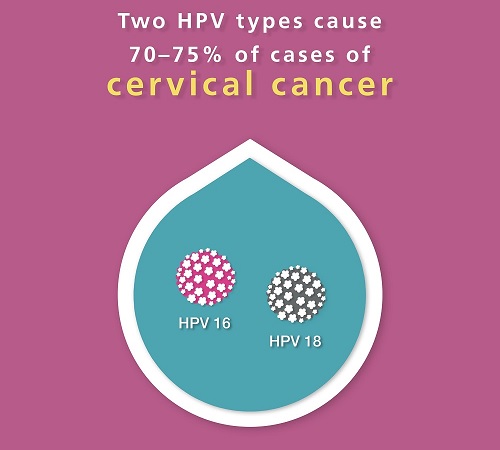
In May 2018, WHO Director-General Dr Tedros Ghebreyesus made a global call for action towards the elimination of cervical cancer. As a result, 194 countries collectively resolved to end needless suffering from cervical cancer, a cancer that the world can eliminate because it is both preventable and curable. IARC has been at the forefront of research to establish the causal role of infection with oncogenic human papillomavirus (HPV) types in cervical cancer, evaluate the safety and efficacy of HPV vaccines, and identify simplified alternatives for screening in low- and middle-income countries.
Below is a selection of content related to IARC’s research on HPV, cervical cancer screening programmes, and understanding the global burden of cervical cancer.
Global strategy to accelerate cervical cancer elimination Digital atlas of visual inspection of the cervixRead news item: Launch of digital atlas of visual inspection of the cervix with acetic acid for screening, triage, and assessment for treatment
HIV-attributable cervical cancer burdenRead news item: Estimates of the global burden of cervical cancer associated with HIV
IARC YouTubeIARC Cervical Cancer YouTube playlist
| Watch playlist |
Cervical Cancer Awareness Month 2020
Cervical Cancer Awareness Month 2020
Interview: Dr Groesbeck Parham
World Cancer Day 2019: Dr Groesbeck Parham to present IARC Cancer and Society Lecture

On World Cancer Day 2019, the 6th International Agency for Research on Cancer (IARC) Cancer and Society Lecture will be presented by Groesbeck Parham, MD. Dr Parham is a professor in the Department of Obstetrics and Gynecology at the University of North Carolina at Chapel Hill, USA. His lecture, “Catalysing a shift in cancer control in a low-resource setting by using what’s available”, will be live-streamed on the IARC website at 11.00–12:00 Lyon time (CET) on 4 February 2019.
With his team, Dr Parham was among the first to provide cervical cancer screening and treatment services on a broad scale to HIV-positive women in sub-Saharan Africa. A leader in cervical cancer prevention in resource-constrained settings, he has collaborated closely with the Zambian Ministry of Health to develop strategies for human papillomavirus (HPV) vaccination countrywide, including a pilot programme to vaccinate 25 000 girls through a school-based approach.
Dr Parham is an adviser to major public health organizations and campaigns, such as the World Health Organization (WHO), the Joint United Nations Programme on HIV/AIDS (UNAIDS), the United States President’s Emergency Plan for AIDS Relief (PEPFAR), and the Pink Ribbon Red Ribbon initiative led by the George W. Bush Institute. Dr Parham collaborates with IARC on projects to study disparities in breast cancer outcomes and new cervical cancer prevention techniques in low- and middle-income countries.
Dr Parham describes his projects in low-resource settings.
What projects are you are currently working on?
Our clinical research team in Zambia is collaborating with investigators from the United Kingdom and France to test new approaches to improving cancer care in resource-constrained settings. We are examining the use of virtual reality simulations and gaming technology to enhance and accelerate the surgical training of young gynaecologists. This is funded by the United Kingdom Medical Research Council and is being led by Professor Richard Sullivan of King’s College London. We are also evaluating the implementation of a low-cost, battery operated device that uses heat to destroy precancerous cells on the cervix. This is led by IARC scientists Dr Partha Basu and Dr Walter Prendiville and is funded by the United States National Cancer Institute.
How are your projects addressing the needs of health care professionals and patients in resource-constrained settings?
According to the Lancet Commission on Global Surgery 2030, fewer than 25% of patients in low-income countries have access to safe, affordable, and timely surgery. In reality, many patients end up dying without ever being treated. The major objective of the virtual reality clinical trial is to determine whether a simulation platform, constructed using low-cost computer equipment, can improve the surgical proficiency of novice surgeons in Zambia.
Improvements in technology are also under investigation in the second trial. One of the major barriers to the expansion of cervical cancer prevention in settings of extreme poverty is the expense associated with the equipment that is used to treat precancerous lesions of the cervix once they are detected. There is a critical need for treatment devices that are not only effective but also portable, low-cost, and easily used by non-physicians. By evaluating these properties in a new device and comparing results to standard methods of treatment, we can find options that could offer solutions to people living in remote, poor, or underserved areas.
What are the next steps needed to improve cancer control and patient outcomes in these areas?
There are three things we can do right now. Firstly, we can introduce massive grass-roots education campaigns about the nature of cancer as well as how it can be prevented and treated. Secondly, substantial financial investment is required in prevention, treatment infrastructure, and management systems. Finally, by using expert advice to correctly implement the things we already know in a comprehensive and extensive way, we could make a huge difference to cancer control, greatly improving patient outcomes.
Interview: Dr Eva Kantelhardt
World Cancer Day 2019: Dr Eva Kantelhardt to present “Breast cancer health service in Ethiopia: insights from cancer registration to long-term care”

For World Cancer Day 2019, the International Agency for Research on Cancer (IARC) has invited Dr Eva Kantelhardt to present a seminar on her work.
Her presentation on “Breast cancer health service in Ethiopia: insights from cancer registration to long-term care” will be live-streamed at 14:00–15:00 Lyon time (CET) on 4 February 2019, World Cancer Day.
Dr Kantelhardt is a clinical gynaecologist and epidemiologist at Martin Luther University of Halle-Wittenberg, in Germany. She works with health care professionals in Ethiopia and other African countries to improve women’s health in underserved areas of the world. Her collaborations have led to transnational projects focused on improving patient outcomes and addressing disparities through an interdisciplinary and holistic approach to women’s health, and female cancers in particular. Her work includes studies on epidemiology, risk factors, and the social determinants of health. Dr Kantelhardt is the Research Coordinator of the African Cancer Registry Network (AFCRN), which is a network Regional Hub for cancer registration in sub-Saharan Africa, in the framework of IARC’s Global Initiative for Cancer Registry Development (GICR).
IARC asked Dr Kantelhardt for an overview of her projects and the impact they are having.
What projects are you currently working on?
Our current projects on breast cancer focus on the unique breast cancer biology in Africa, the implementation of endocrine treatment, and optimizing patient referral linkage – the process of ensuring that people who screen positive for disease receive treatment and follow-up. A population-based trial comparing different methods of cervical cancer screening, which evaluates uptake of screening and adherence to procedures among other aspects, is also under way.
The Addis Ababa City Cancer Registry, a population-based registry that has been active since 2012, is a project that is run in close collaboration with the AFCRN and IARC. Apart from hospital-based outcome studies, we are also interested in cancer care in rural areas.
What are the main challenges you and your colleagues face in areas where health services are limited?
There is a serious lack of trained staff, such as oncologists and surgeons. Health services and patients have limited financial resources. The need for interdisciplinarity, closer communication, and improved links between cancer care institutions also presents specific challenges.
How do your projects address the needs of health care professionals and patients in underserved areas?
We have implemented a training programme for gynaecologic oncologists in Ethiopia, increasing the number of these specialists in the country from 2 to 6, with another 10 in training. These gynaecologists each perform about 10 major abdominal surgeries for ovarian, cervical, or vulvar cancer every week.
To improve laboratory capacity, we have trained five colleagues in human papillomavirus (HPV) testing and determination of breast cancer hormone receptor status. This has allowed about 3000 women to be screened for cervical cancer and about 10 000 to be screened for breast cancer, and about 1500 breast cancer patients have received information on their hormone receptor status. Projects like this serve patients in need by providing endocrine treatment for breast cancer patients at no cost, and by increasing the capacity for cervical cancer screening.
Since 2014, we have been supporting lectures and continuing medical education sessions on gynaecologic cancer at the annual meetings of the Ethiopian Society of Obstetricians and Gynecologists, and since 2012 there have been annual oncology conferences.
Our projects have also supported 15 oncology residents in their mandatory final-year research, 10 of whom have now graduated. A total of 25 German MD students, about 20 Ethiopian master’s students, and 10 Ethiopian PhD candidates have been jointly supervised and supported financially to perform research on cancer in Ethiopia and other African countries. Improved cancer data assist members of the AFCRN, part of the IARC-led International Association of Cancer Registries, who also collaborate with the American Cancer Society.
Together with the Addis Ababa University School of Public Health, we have developed a curricular module on noncommunicable diseases, including cancer, for master’s students there. This will ensure improvement of health services in rural areas and primary health care services overall.
What are the next steps needed to reduce disparities and improve patient outcomes in these areas?
The main driver for success seems to be political commitment. Investments, such as in radiotherapy, can only come from governments. Cancer control programmes must guide an interdisciplinary approach, including all levels of health service. Downstaging – the ability to decrease the size or number of cancerous tumours at diagnosis to a less threatening stage – and access to guidelines to standardize therapy will also hopefully improve outcomes for patients.
Posters
World Cancer Day 2019: Posters
 Download |
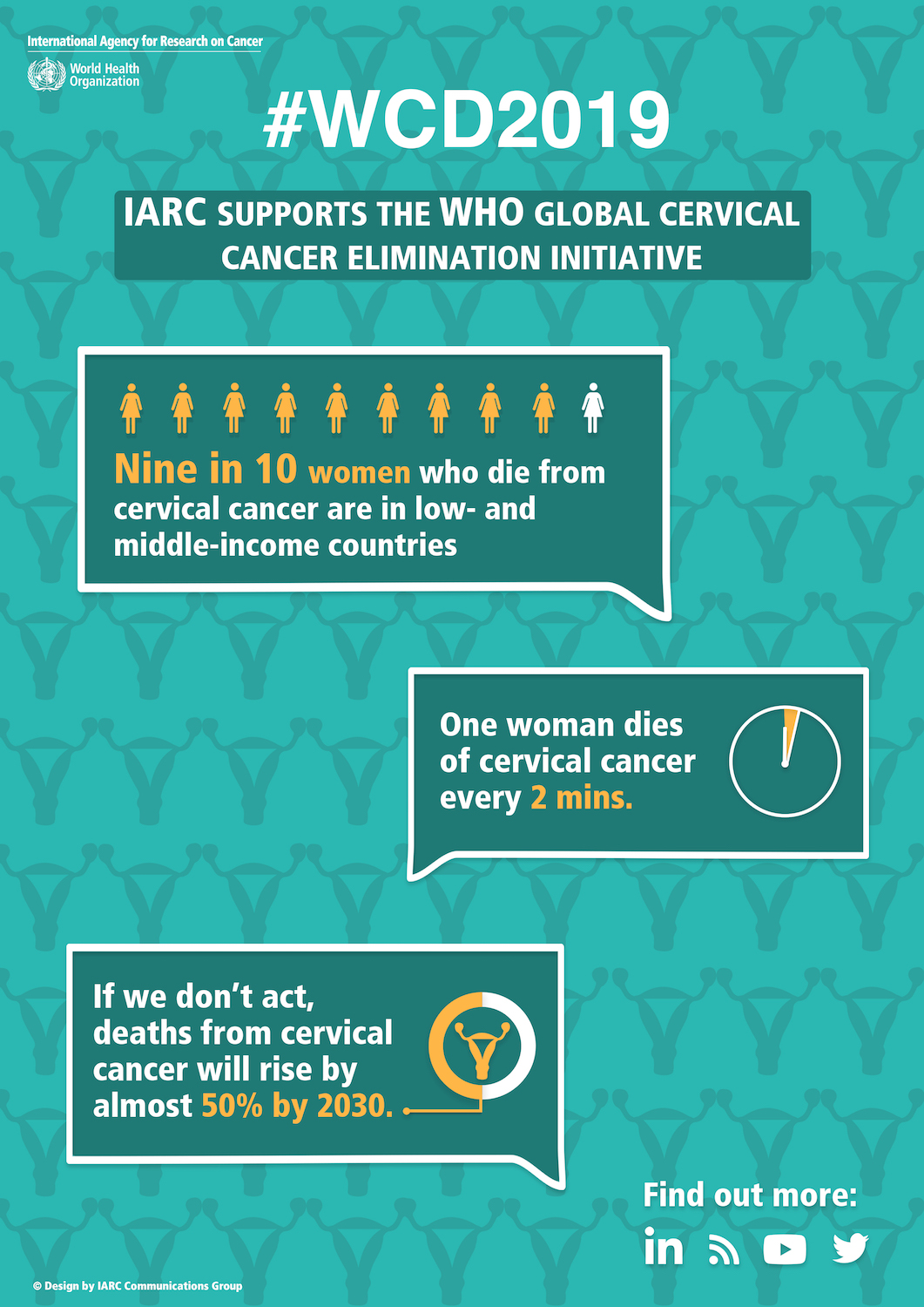 Download |
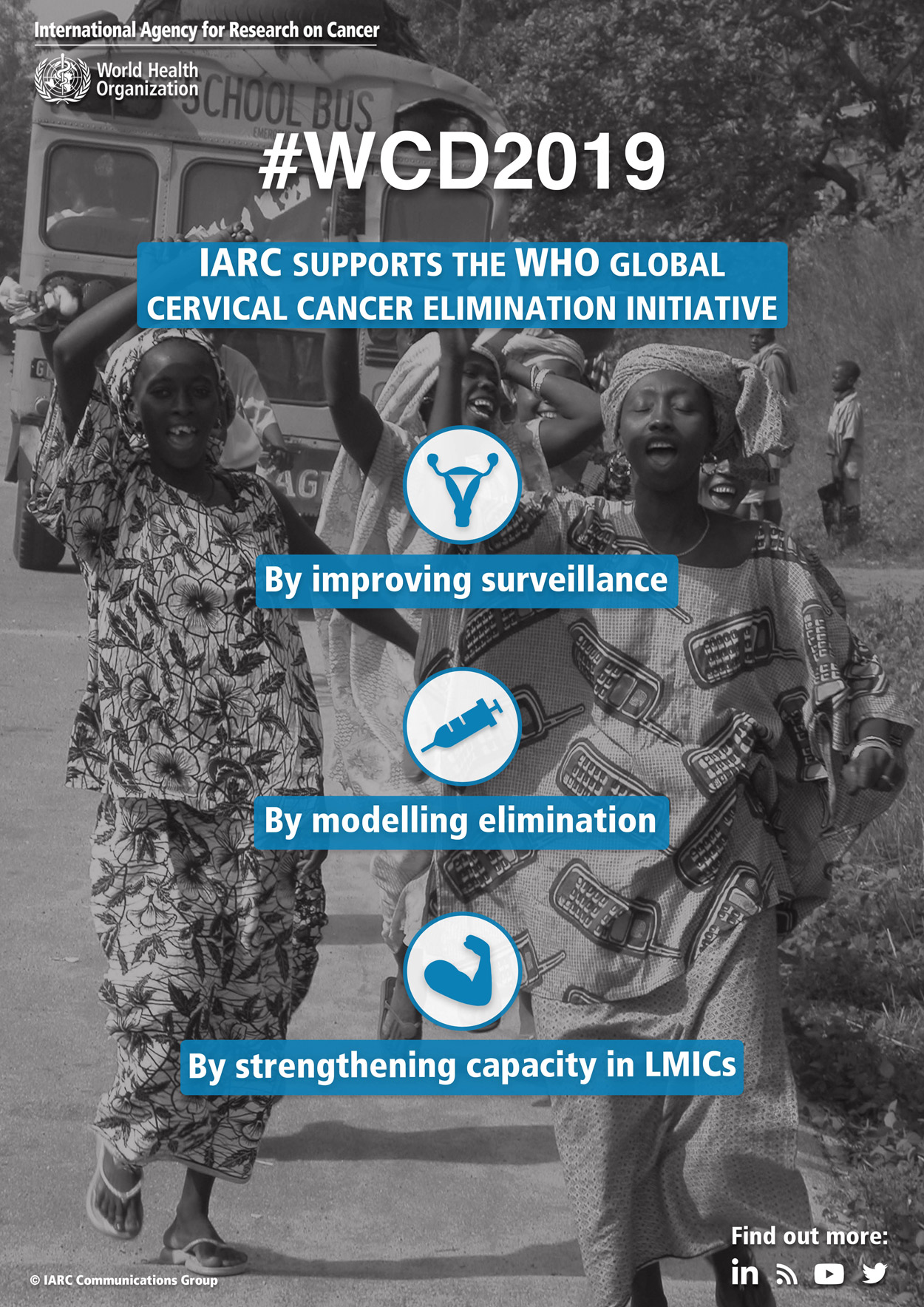 Download |