About
The activities of the Early Detection, Prevention, and Infections Branch (EPR) include a wide portfolio of studies that directly inform national and international policies in cancer control. Such studies include those evaluating etiology and natural history, assessing the global burden of infection-associated cancers, studying the efficacy and effectiveness of cancer prevention and early detection interventions, and evaluating and modelling the impact of interventions. A major theme is evaluating interventions through the lens of implementation science. Carcinogenic infectious agents are particularly amenable to cancer prevention (e.g. vaccines, diagnostic tools, and therapies), and the burden of infection-attributable cancers is disproportionately high in low- and middle-income countries (LMICs) (> 25% of all cancer cases in certain global regions). Therefore, a significant proportion of EPR’s prevention research focuses on infection-related cancers. Evaluating determinants of delays in accessing diagnostic and treatment services for symptomatic patients is a key EPR research focus in LMICs. EPR’s research explores new horizons in cancer prevention research, such as the development and evaluation of artificial intelligence (AI)-based solutions and microbiome analysis. It also explores biomarker-based risk stratification and early detection approaches for high-burden cancers. EPR also supports capacity-building to implement quality-assured public health programmes for cancer prevention and early detection.
Specific aims
- To translate knowledge about cancer etiology and mechanisms into evidence-based interventions that can prevent cancer suffering and death. EPR has a strong focus on prevention of carcinogenic infections, and also emerging obesity-related risk factors and addictive substances such as pharmaceutical exposures and tobacco exposure.
- To evaluate novel strategies for cancer prevention and early detection, with a view to reducing the cancer burden and improving survival and quality of life of patients after treatment.
- To develop and validate risk-based approaches to primary and secondary cancer prevention, including biomarker-informed strategies.
- To support capacity-building in real health-care settings to implement evidence-based interventions in cancer prevention and early detection with high quality and equity.
- To assess the implementability and scalability of context-specific cancer prevention interventions to inform policy decisions through implementation research.
Major approaches/areas of research
The interventions evaluated can be broadly categorized into those relevant to: (i) etiology and primary prevention of cancers associated with carcinogenic infections with established modifiable infectious risk factors (e.g. preventing human papillomavirus [HPV] and hepatitis B virus [HBV] infections through vaccination; screening and treatment of Helicobacter pylori and hepatitis C virus [HCV] infections); (ii) screening of asymptomatic at-risk populations and downstream management for cancer sites for which the current evidence base is more established (cervical cancer, breast cancer, colorectal cancer, oral cancer, and lung cancer) or emerging cancer sites (e.g. gastric cancer, prostate cancer, and anal cancer); and (iii) early diagnosis of common cancers in symptomatic individuals, with a view to shifting the stage distribution of tumours detected towards a lower stage and improving survival and quality of life of patients after treatment. Complementing these intervention-focused activities, EPR conducts large-scale, collaborative epidemiological research to quantify cancer risk associated with emerging risk factors, including obesity-related risk factors and exposures to opioids and pharmaceuticals, as well as tobacco exposure. EPR also has an important focus on developing and validating risk prediction models and biomarkers for translation into targeted prevention of priority cancers, including lung cancer and HPV-driven cancers, as well as for multi-cancer early detection. The evaluation of prevention, screening, and early diagnosis focuses on the effectiveness in various health-care settings and on understanding the related implementation challenges. A core objective across these activities is to translate epidemiological and modelling evidence and outcomes of observational and intervention studies into actionable guidance for public health policy, clinical practice, and cancer control planning.
Etiology and primary prevention of cancers associated with carcinogenic infections
IARC is the global reference for estimates of the burden of infection-attributable cancer. This programme serves to raise awareness, inform recommendations for preventive action, prioritize resources, and monitor the long-term impact of cancer prevention policies that target infectious agents, on both the local and global scales. Current EPR priorities to improve these estimates include establishing the population attributable burden of HIV to cancers (e.g. cervical cancer, Kaposi sarcoma, non-Hodgkin lymphoma, and anal cancer), of hepatitis virus to liver cancer, and of Epstein–Barr virus to non-Hodgkin lymphoma and gastric carcinoma.
HPV vaccination is the main component of the World Health Organization (WHO) global strategy to eliminate cervical cancer as a public health problem. EPR is engaged in evaluating the efficacy of the HPV vaccine and the impact of HPV vaccination programmes in real-life conditions, as well as modelling the impact of HPV vaccination in different implementation scenarios, most notably that of a single dose of HPV vaccine. The evidence guides health policies and supports national authorities in implementing HPV vaccination programmes, particularly in LMICs, in order to reduce global disparities in cervical cancer.
H. pylori infection is the most important cause of gastric cancer worldwide. The ENIGMA studies aim to understand risk factors including H. pylori prevalence in diverse populations with variable gastric cancer risks using standardized multicentre protocols. The Meta-GC and INTL-CC projects investigate pre-diagnostic metabolite signatures for gastric cancer development prospectively in samples using large cohort studies. In anticipation of results from ongoing research (the HELPER trial), which are expected to establish the preventive effect of screening and treatment of H. pylori for gastric cancer, EPR is expanding research into the implementation of such programmes, for example in Europe, both by undertaking operational research in programmatic settings in LMICs and by leveraging expertise in modelling the natural history of carcinogenic infections to inform national and international recommendations (EUROHELICAN, TOGAS, IARC Working Group Report No. 12, and EC-GaC). EPR is engaged in supporting countries through evidence-based implementation guidance in this emerging area of gastric cancer prevention.
EPR is studying the association of the vaginal microbiome with the natural history of cervical cancer and its role is predicting disease progression and response to treatment of cervical precancers, especially in women living with HIV.
Etiology and primary prevention of emerging, addictive, and pharmaceutical exposures
EPR conducts research on emerging, addictive, and pharmaceutical exposures with potential relevance for cancer risk, addressing important evidence gaps for widely used substances whose carcinogenic potential remains insufficiently understood. Prescription opioids represent a potentially important group of emerging cancer risk factors, with growing epidemiological evidence suggesting associations with cancers of the lung, pancreas, bladder, and oesophagus. Despite their extensive and long-term use, particularly in the context of the global opioid crisis, the carcinogenic potential of prescription opioids remains poorly understood.
To address this gap, EPR coordinates the Opioid Cohort Consortium (OPICO), which brings together data from 28 sources across the USA, Europe, Asia, and Australia, including prospective cohorts, medication dispensing/prescription databases, and cancer registries. By harmonizing data from nearly 2 million individuals and applying advanced epidemiological methods, OPICO aims to quantify cancer risks associated with opioid use across multiple cancer sites. This work builds on IARC’s long-standing research that led to the classification of opium consumption as carcinogenic to humans (Group 1) by the IARC Monographs programme (Volume 126).
Obesity is an established carcinogen, accounting for at least 4–8% of global cancers, and is expected to overtake smoking as the leading cause of cancer in some countries. Through the Obesity-related Cancer Epidemiology Programme (OCEP), EPR investigates how obesity and its biological effects contribute to cancer risk, with a focus on molecular mechanisms, pharmacoepidemiology, and the cancer-preventive potential of anti-obesity medications. This work supports the development of targeted, risk-based prevention strategies for obesity-related cancers.
In parallel, EPR is expanding research on the use of other addictive substances with increasing population exposure, including waterpipe and cannabis smoking, chewing tobacco, and using electronic cigarettes. Using established international collaborations and epidemiological infrastructures, this work aims to generate evidence on potential cancer risks associated with these exposures.
Screening of asymptomatic at-risk populations
EPR is conducting a range of studies that evaluate new technological innovations in cancer screening and management of premalignant conditions and assess their suitability and applicability for implementation, in particular in limited-resource settings.
To accelerate the introduction of HPV-based screening, in alignment with the WHO Cervical Cancer Elimination Initiative, the IARC portfolio on cervical cancer screening includes: evaluation of novel HPV detection tests (detection of high-risk HPV E6/E7 oncoproteins, detection in urine using polymerase chain reaction (PCR)-based technologies and AI-assisted infrared spectroscopy); techniques for triage of HPV-positive women (using methylation tests in cervical and urine samples); HPV screen-and-treat programmes in Africa, with a particular focus on women living with HIV; and randomized controlled trials in Zambia and India on the efficacy, safety, and cost–effectiveness of cervical thermal ablation. The EASTER and SAVE-CERVIX multicentre studies are developing and validating AI algorithms to detect cervical neoplasia in HPV-positive women and also assessing the ethical and legal dimensions of routine use of AI.
A multicentre study to evaluate the use of portable ultrasound to triage women positive on clinical breast examination (CBE) for breast cancer screening in India, Morocco, and Indonesia will generate valuable evidence on the efficacy of ultrasound triage to improve the positive predictive value of CBE. EPR co-leads clinical trials that combine H. pylori eradication with endoscopic surveillance to reduce gastric cancer incidence and mortality (the HELPER and GISTAR trials).
EPR is also conducting a range of studies to understand the major barriers to accessing quality-assured cancer screening, and to evaluate interventions directed at multiple levels (systems, providers, and clients) to increase participation. The Cancer Screening in Five Continents (CanScreen5) project evaluates the quality and organization of cancer screening programmes globally. CanScreen5 has a strong focus on building capacity in countries to be able to implement quality-assured and evidence-informed cancer screening programmes. EPR’s implementation research studies aim to document the challenges that countries face while introducing major changes in their existing screening programmes (e.g. transitioning from cytology-based to HPV-based cervical cancer screening) and suggest context-appropriate solutions. A major scope of EPR research is developing the European guidelines on HPV vaccination, cervical cancer screening, gastric cancer screening, and quality assurance.
With the recent European Commission recommendation to extend organized screening to three additional cancer types – lung cancer, prostate cancer, and gastric cancer – EPR is also involved in major related implementation studies in Europe (PRAISE-U for prostate cancer and TOGAS and EUROHELICAN for gastric cancer).
For prostate cancer, EPR led a work package to develop context-appropriate risk-stratified screening protocols and related key performance indicators for implementation pilots in five European Union (EU) regions through the PRAISE-U project. EPR researchers are also extending the learnings of the PRAISE-U project to an additional site in Slovenia (ProScreen project). EPR is entrusted with preparing periodic reports on the status of implementation and performance of breast, cervical, colorectal, and lung cancer screening programmes in the EU.
For gastric cancer, EPR plays a major role in assessing the implementability of population-based H. pylori screen-and-treat programmes for gastric cancer prevention (EUROHELICAN) and providing missing knowledge for recommending appropriate implementation of gastric cancer screening across Europe (TOGAS). EPR is also leading the European Commission Initiative on Gastric Cancer (EC-GaC), which aims to develop the first European guidelines and prepare a quality assurance scheme for gastric cancer prevention.
EPR is also advancing biomarker-based early detection of HPV-driven cancers by developing and validating blood-based markers, including HPV-related antibodies and circulating HPV DNA, to support risk-stratified screening and improved triage strategies.
For lung cancer, EPR conducts integrated research on risk-based screening and prevention, combining individual- and population-level risk stratification, biomarker development, and impact modelling. Leveraging international cohort data and national screening initiatives, including the Lung Cancer Cohort Consortium (LC3), this work generates evidence to inform targeted screening strategies, smoking cessation interventions within screening and oncological care, and policy-relevant implementation integrating prevention and risk-based screening to reduce lung cancer incidence and mortality.
For multi-cancer screening, EPR plays a role in addressing the emerging field of multi-cancer early detection tests (MCEDs) by evaluating the evidence base for blood-based screening tests, including the assessment of alternative trial end-points and the development of risk-based strategies to guide targeted and equitable implementation. This will involve developing standards of evidence within the OVERCAST project, which will evaluate proposed alternative trial end-points (e.g. reductions in late-stage cancer incidence) as potential surrogates for mortality using data from 15 randomized cancer screening trials. In parallel, EPR will develop strategies for efficient implementation of MCEDs by targeting individuals who are most likely to benefit using risk-based strategies based on multi-cancer risk models.
Early diagnosis of common cancers
To better understand the challenges in implementing cancer early diagnosis and the means to improve it, in particular in LMICs, EPR is evaluating barriers to accessing timely diagnostic and treatment services for symptomatic individuals, including measuring delays across the cancer care pathway and their determinants, and identifying setting-appropriate solutions to minimize such barriers and delays (Access Cancer Care India study, the DECAN project in Nepal, and patterns-of-care studies in Egypt, Morocco, Iraq, and India). A major component of these studies is evaluation of quality of life during various phases of the cancer journey. Measuring the delays in access to early diagnosis in paediatric patients with cancer and assessing their determinants and impact on quality of life and survival (DECAN-CHILD project in Nepal) is a major focus of EPR.
EPR is conducting studies that identify relevant gaps in the health systems across the cancer care continuum and suggest contextualized and sustainable solutions. Keeping pace with the advancement of technology, EPR is assessing the applicability of new technology: mobile technology with AI-powered chatbots to educate the community, the use of mobile phone-based applications for patient navigation, and the web-based promotion of telepathology and distance learning for service providers.
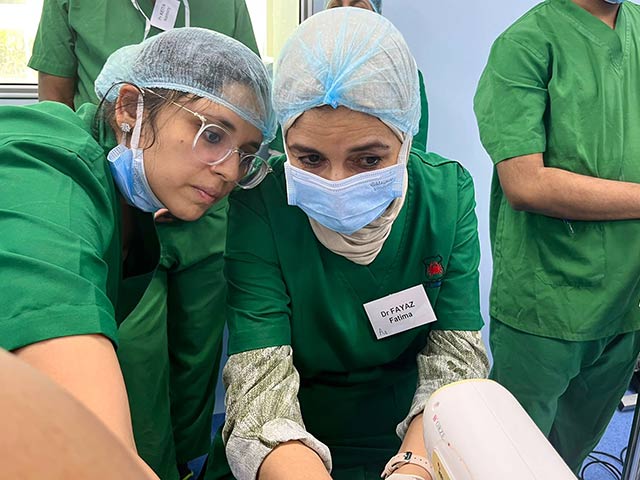
Furthermore, through collaboration with ministries of health in several countries (priorities for LMICs), EPR assists them in planning and implementing quality-assured cancer control programmes, including training of health professionals and researchers in the field of cancer prevention.